S.N. Navruzov, S.B. Abdujapparov, B.S. Navruzov
Republican Research Oncology Center of the Ministry of Public Health,
Republic of Uzbekistan
ABSTRACT
AIM
There are no precise recommendations for the application of concrete types of sutures and suturing materials in various location of colorectal cancer. This study aimed to optimize the using of circular suturing devices and dissection of lymph nodes in surgical treatment of colorectal cancer.
PATIENTS AND METHODS
Patients to be treated with sphincter-preserving operations were divided into 3 groups. Group I included 29 (35.4%) patients with tumor located at 10-15 cm away from the edge of dentate line. Patients from this group were treated with anterior resection of rectum with anastomosis and standard lymph nodes dissection. The group II had 18 (21.9%) patients with the tumor located at 9 cm or lower from dentate line. These patients were treated with low anterior resection with anastomosis and extended lymph nodes dissection. The (control) group III enrolled 35 (42.7%) patients with various location of the tumor in rectum. Control group patients were treated by abdomino-anal resection of rectum with standard lymph nodes dissection (19 patients with pulling proximal parts of colon into anal canal and 16 patients with pulling sigmoid colon into anal canal). Reconstructive recovery stage was carried out as one step in 56 patients and in two steps in 26 patients.
RESULTS
There are significant differences regarding the short-term effects of these three groups, such as post-operative complications: suppuration of post-operative wound, incompetence of anastomosis, acute adhesive intestinal obstruction, bleeding, necrosis, and retraction of pulling colon. Two study groups were much better than the control group. The long-term effects manifested by the three-year survival rate in group I, II and III were 82,8% (p=0.0084), 77.8% (p=0.091) and 65.7% respectively. Quality of Life scales are higher for group I and II than group III.
CONCLUSION
Low anterior resections with extended lymph nodes dissection demonstrated to be superior to abdomino-anal resection of rectum in following indices: decrease of the local recurrences, prolongation of life duration, improvement of physical and psychological status.
KEYWORDS
rectal cancer, circular suturing devices, anterior resection of rectum, abdominal-anal resection of rectum, lymph nodes dissection
Introduction
Incidence of rectal cancer (RC) is increasing in many countries for last decades. About 50 new cases of colorectal cancer per 100, 000 population is reported every year, this number presents a 5% risk to develop this disease during one’s individual life [5]. Surgical treatment of RC with adherence to the principles of radical removing of the tumor is a main and the most efficient curative method [1, 9].
For a long time, extirpation of the whole organ, including all the structures of obtrusive apparatus, in any location of the tumor in the rectum, dominated in oncology protocol. Many researches of lymph outflow from rectum have changed this concept. It was established that lymphatic fluid from rectum outflows mainly into two directions. If we conventionally divide rectum by a transversal plane at the level of 6 cm from the edge of the anus, lymph fluid from the parts below this plane (anal canal, low ampullary part) outflows in the direction of medial and inferior rectal vessels, i.e., downwards, and aside). Main regions of metastatic cancer cells spreading along with pararectal lymph nodes are inguinal, pelvic, and iliac lymph nodes. From the parts localized above 6 cm (medial and superior ampullary parts), lymph outflows along superior rectal vessels, so the tumor in such location is not necessity to remove the anus, cross levator portions and conduct wide extirpation of pelvic fat [7,17].
Recent years a tendency to expansion of indications for organ preserving operations in RC is observed. It is necessary to develop clear criteria to evaluate their performing based on comparative analysis of remote results of the treatment, for example, the frequency of regional recurrences. Mastering and introduction of methods with application of suturing devices and substantiation of indications to use combined and complex curative programs will increase the efficiency and ablativity of surgical interventions [11, 12, 16, 17].
Incompetence of anastomosis is one of the most dangerous complications in coloproctology and it is registered in 5-6% of all cases. Lethality of this complication is high: up to 50-69%. Prevention of incompetence of anastomosis is of great interest to surgeons [2, 6].
Currently double-row suture is used frequently in colorectal surgery. In such cases anastomosis healing takes place by second intention, the numbers of incompetence average 13-16%. Single-row sutures provides healing by first intention, the numbers of incompetence of anastomosis formed by single-row continuous suture averages from 0 to 3.4% [3, 4].
Development and introduction of special suturing devices permitting to form colorectal and coloanal anastomosis under topographically unfavorable conditions of small pelvis can be considered as a revolutionary achievement in coloproctology. This method of forming colorectal anastomosis practically lack shortcomings common to traditional methods and can be used successfully in surgical treatment of RC. Mechanical suture induces minimal trauma in connected parts, contributes a tight adherence of their edges. Titanium staples don’t induce damage of adjacent tissues. Incompetence of anastomosis occurs in 1.9-6.4% of all cases [3, 11].
Many studies on comparison of manual and mechanical sutures in colorectal surgery don’t give an unequivocal answer: which suture is better. Some authors prefer mechanical suture [6,10], others emphasize advantages of manual suture, especially single-row variants [8,14]. Numbers of surgeons consider mechanical and single-row sutures as identically acceptable in colorectal surgery [4, 17].
There are no precise recommendations for application of concrete types of sutures and suture materials in various localization of tumor and stage of the disease. Thus, a present tendency to increasing of RC morbidity, high level of postoperative lethality, development of frequent recurrences and metastatic spreading, low indices of 5-year survival of patients, unsatisfactory quality of patients’ life, difficulties in social and labor rehabilitation demonstrate the necessity of investigations with the aim of optimization of RC surgical treatment.
Patients and methods
Eighty-two patients with RC in stage II-III of the disease (stages B and C by Dukes) were treated (table 1). Results of the operative treatment using anterior and inferior anterior resection of rectum with standard or extended lymph nodes dissection and forming colorectal anastomosis with the aid of circular suturing devices (CSD) were studied. Methods of investigation included rectoscopy, colonfibroscopy, irigography, proctography, morphological studies, immunohistochemistry, computer tomography examination of small pelvis organs.
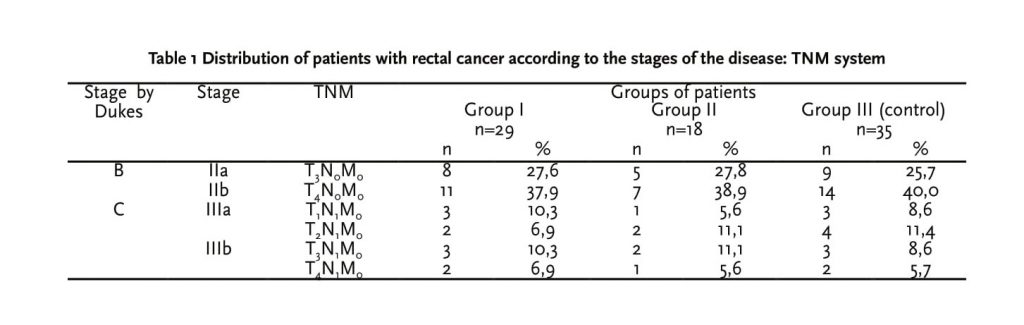
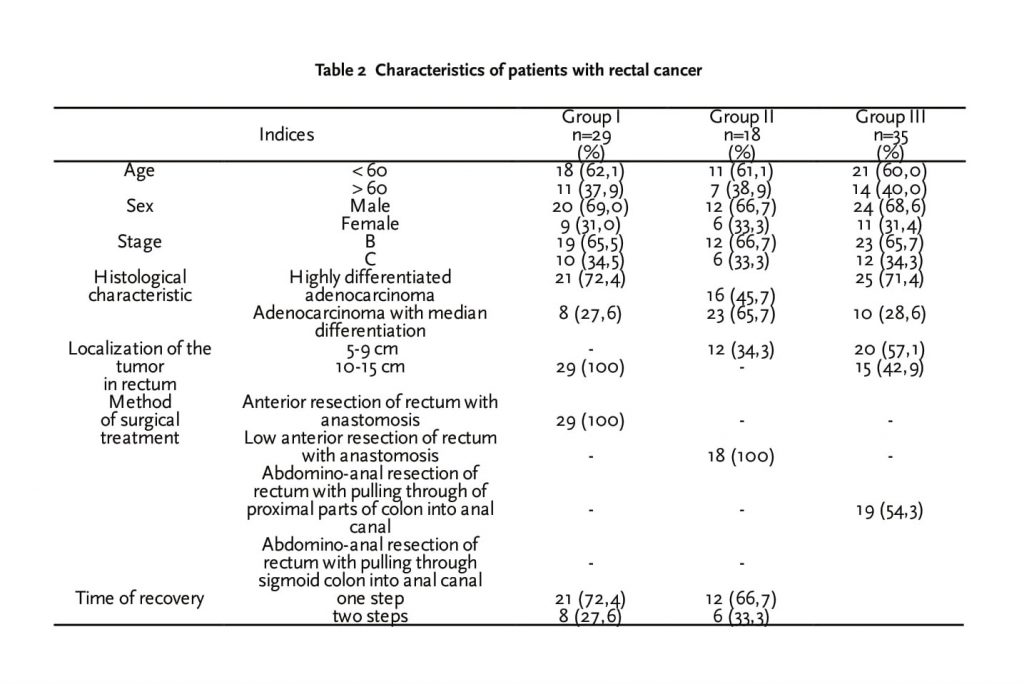
Patients with sphincter-preserving operations were divided into 3 groups. The group I included 29 (35.4%) patients with tumor localization at 10-15 cm distance from the edge of dentate line (table 2). These patients were treated with anterior resection of rectum with anastomosis formed by CSD with standard lymph nodes dissection. The group II included 18 (21.9%) patients with the tumor located at 9 cm or lower from dentate line. These patients were treated with low anterior resection with anastomosis formed by CSD and extended lymph nodes dissection. The (control) group III included 35 (42.7%) patients with various location of the tumor in rectum. Control group was treated by abdomino-anal resection of rectum with standard lymph nodes dissection (19 patients with pulling proximal parts of colon into anal canal and 16 patients with pulling sigmoid colon into anal canal). Reconstructive recovery stage was carried out as one step in 56 patients and in two steps in 26 patients. There were 56 men and 26 women; average age of the patients was 56.4 years. Highly or moderate differentiated adenocarcinoma was diagnosed morphologically in all the patients.
Results
Short term effects of the treatment
At the short period of post-operation, complications were observed in 4 patients in the group I and group II (table 3). Partial incompetence of colorectal anastomosis was diagnosed in 1 patient on the 5th day after operation. Conservative measures were efficient and on the 15th day manifestations of incompetence were stopped and the patient was discharged from the hospital for the treatment at a polyclinic. Suppuration of post-operative wound was observed in 3 patients, antibiotics and local conservative procedures were applied.
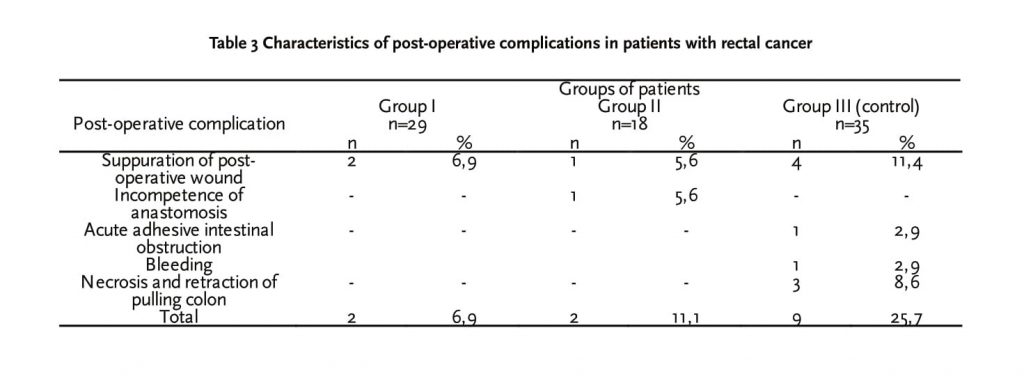
Suppuration of post-operative wound was observed in 4 patients received conservative treatment. Acute adhesive intestinal obstruction developed in 1 patient and bleeding from post-operative wound took place in 1 patient. Necrosis and retraction of pulling colon was registered in 3 patients. Above mentioned complications were treated with surgical methods. Colostoma was carried out in necrosis and retraction of pulling colon.
Morphological examination showed that metastatic lymph nodes existed in 3 patients (up to 3 lymph nodes). Metastases in more than 3 lymph nodes were found in 2 patients. Immunohistochemical methods (staining for cytokeratins) revealed metastases in lymph nodes in 7 patients in the group I and group II. In the control group (group III), metastases in lymph nodes were found in 5 patients. Examination of the incision line didn’t reveal residual tumor cells. Patients with metastases in lymph nodes received chemotherapy with standard adjuvant regimen FOLFOX-4.
Long term effects of the treatment
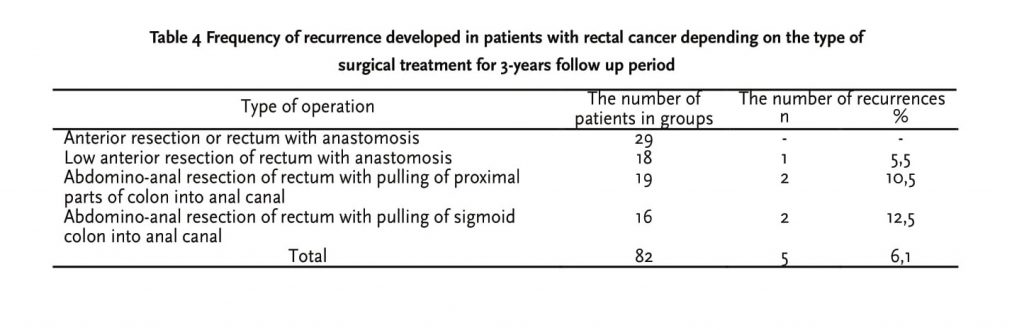
After anterior resection of rectum with standard lymph nodes dissection, recurrences of cancer were not observed in the group I patients in 3 years’ follow up period (table 4). One case of the tumor recurrence after low anterior resection of rectum with extended lymph nodes dissection was observed in group II.
Within 3 years’ follow up duration, 4 (11.4%) cases of recurrences were observed in the control group. Two of them developed after pulling proximal parts of colon into anal canal, and another 2 patients developed after pulling sigmoid colon into anal canal.
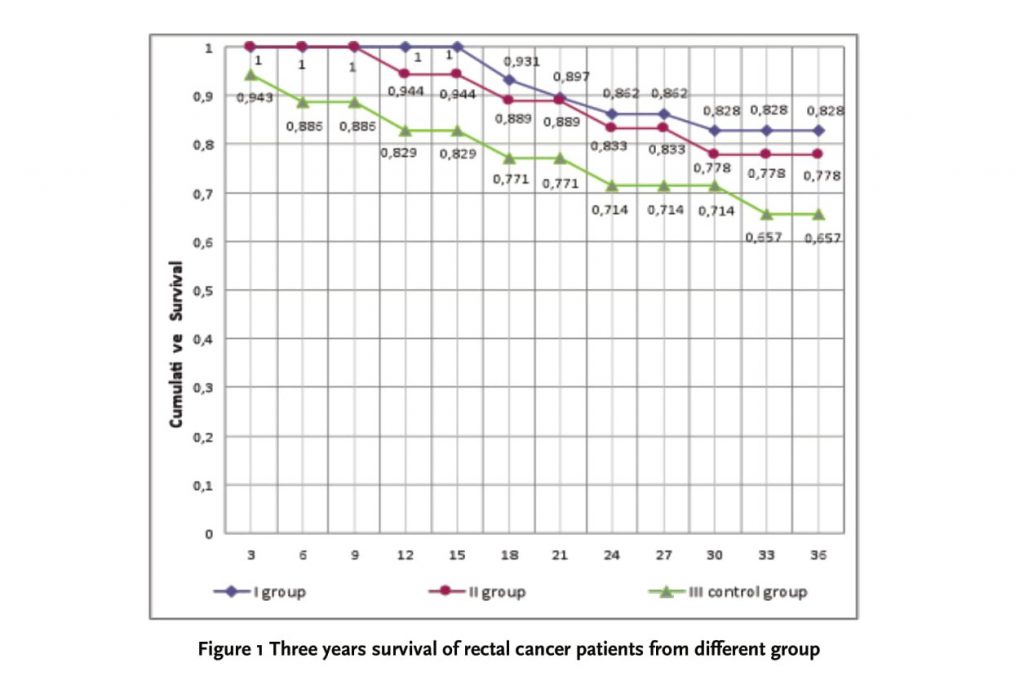
The three-year survival rate in RC patients received different surgical treatment in group I, II and III were 82,8% (p=0,0084), 77,8% (p=0,091) and 65,7% (fig. 1) respectively.
Study of quality of life
Quality of Life of the patients with RC after surgical treatment was estimated by questionnaire Medical Outcomes Study36-Item Short-Form Health Survey (MOS SF-36) [13], and also with questionnaire for estimation of severity of gastrointestinal symptoms (Gastrointestinal Symptom Rating Scale (GSRS) [15].
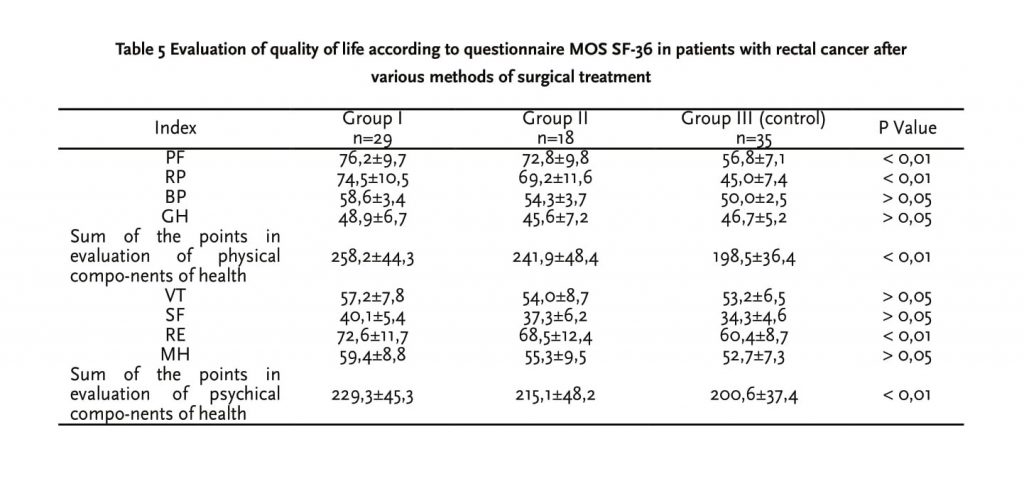
Comparative results of study of quality of life in patients with the aid of questionnaire MOS SF-36 are shown in table 5.
Significantly higher summary indices of physical and psychological health in patients with anterior resection of rectum in comparison with the group with abdomino-anal resection of rectum were found. The maximal differences were expressed in evaluation of physical health. Differences in indices between groups of patients with standard and low anterior resection were minimal.
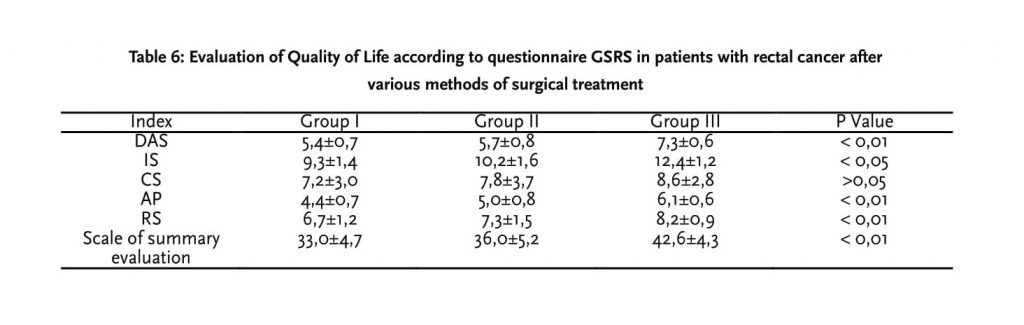
To explore more detailed characteristics of Quality of Life, which is connected with post-operative changes in abdominal cavity after various methods of surgical treatment, we compared appropriate indices of gastroenterological questionnaire GSRS (table 6).
All five scales of specialized questionnaire (less values reflect better results) showed significant evidence of better Quality of Life by the state of organs in abdominal cavity in patients underwent anterior resection of rectum in comparison with abdomino-anal resection of rectum.
Discussion
In our clinic, as a consequence of evolution of viewpoints at oncological and functional expediency of surgical intervention in rectal cancer, abdomino-perineal extirpation, the gold standard, is now becoming replaced by sphincter-preserving resections. Approaches of resection were also undergoing a number of changes. According to our data, tumors located out of the zone of the obtrusive apparatus of rectum have been observed in more than half of patients, which means that in most cases, there are prerequisites to preserve obtrusive apparatus in adherence to the principles of radical tumor extirpation.
One of the actual imperative problems in colorectal surgery is the implementation of sphincter-preserving operation in patients with tumor located in median and inferior ampullary parts of the rectum, adhering to the principles of oncology radicalism. There are following problems in such situations:
1. Low functional indices after traditional operative methods in cancer located in low ampulla of rectum.
2. Many postoperative complications after abdominoanal resection of rectum with pulling through (suppuration of presacral zone, necrosis, and retraction of a pulling colon).
3. Undifferentiated approach to lymph nodes dissection results in an increased tumor recurrences.
4. Technical impossibility to form manual colorectal anastomoses in low and ultralow stumps of rectum after its resection.
Anterior resection of rectum with standard lymph node dissection was fulfilled in 29 patients. In anterior resection, we stepped back from the inferior edge of the tumor no less than 5 cm, and from the superior pole from 12-15 cm. After resection of the affected segment of rectum and a part of the sigmoid colon, we formed colorectal anastomosis of the type “end to end” with the aid of CSD. Devices of the firms “Autosuture” and “Ethicon” are very reliable. Using the technique of double stapling anastomosis, consisting of the rectal stump stapling by a linear suturing device and then forming colorectal anastomosis “end to end” by CSD, implementation of low anterior resection with anastomosis localization 1-2 cm higher from the dentate line is rather easy. Irrespective of the method of anastomosis forming its safety was checked by blowing out the colon with air.
Anterior resection of rectum is contradicted to patients with intestinal obstruction. In this case, we carried out Gartman’s operation (complete stapling of rectal stump and forming of colostoma on the anterior abdominal wall). It is possible also abdomino-anal resection of rectum with colostoma when the colon instead pulling into anal canal is taken out on the anterior abdominal wall as colostoma. Final volume and type of operative intervention were detected after laparotomy and careful revision of organs in abdominal cavity. As a rule, median incision was used, permitting to examine all the parts of abdominal cavity and retroperitoneal space and perform any type of operative intervention without technical difficulties.
Preference to anterior resections is associated with an opportunity to put a formed anastomosis retroperitoneally. It prevents infection of abdominal cavity in the development of incompetence of anastomosis. decompression of colon after such operations are accessible and easily to be implemented, which is of importance for anastomosis healing.
Implementation of low anterior resection in tumors localized 5-9 cm from the dentate line is potential by the development of surgical technique and new generation of CSD. This comparatively new operation is introduced insufficiently in practice of surgical hospitals, first of all, due to the difficulties in its implementation. We carried out this operation only after careful examination, including US scanning, and excluding lymphogenic metastatic spreading in mesorectum. We carried out simultaneously an extended lymph nodes dissection.
An important aspect for selection of indications for various types of sphincters preserving operations in cancer of inferior and median ampulla parts of rectum is a possibility of adequate lymph nodes dissection, especially lymph nodes along medial intestinal arteries. Adequate lymph nodes dissection with allowance for main pathways of lymph outflow is the most important factor of prophylaxis of regional recurrences. Taking into consideration that main pathway of lymph outflow from tumors in these parts of rectum directs along superior rectal vessels, the latter must be ligated in the place of their separation from inferior mesenterial artery (or from sigmoid artery) and removed with the tumor in a single block. If enlarged lymph nodes along inferior mesenterial artery are found, the latter is ligated in the place of its separation from aorta. Blood supply of the rest part of the sigmoid colon is accomplished at the expense the arc of Riolan. In the case of inadequacy of blood supply of sigmoid colon left flank of the colon is mobilized with forming of transverse-rectal-anastomosis.
Anterior resection and abdomino-anal resection of rectum are of comparable radicalism on condition of removal of lymphatic collectors along median intestinal arteries. In the cases when anterior resection lateral ligaments are not mobilized (i.e., when total mesorectumectomy is not performed), the volume of lymph nodes ectomy is less adequate in comparison with abdomino-anal resection. So, in metastatic affection or in suspicion to metastases we preferred abdomino-anal resection.
Abdomino-anal resection in control group was carried out by two teams of surgeons: abdominal and perineal. Perineal team dissected all the layers of intestinal wall through transanal passage as far as connection with abdominal team of surgeons. The operation was finished by one of the methods: 1) pulling of proximal parts of colon into anal canal (19 patients), 2) pulling of sigmoid colon into anal canal (16 patients). Lymph nodes dissection in standard volume was carried out simultaneously in all the patients. Selection of the method for finalizing the operation depended on the state of a patient, intensity of perifocal inflammation, other complications, for example, disorders of intestinal patency.
Abdomino-anal resection of rectum with additional resection of superposed parts of colon belongs to the category of very complicated interventions due to topographical peculiarities of rectum and necessity of manipulations in the depth of small pelvis. The main danger of these operations is a possibility of infection of small pelvis cavity in mobilization of rectum by perineal team of surgeons. Perineal wound is easily infected and minimal errors during operations usually induce pro-inflammatory changes in small pelvis cavity.
Surgical intervention in uncomplicated course of cancer in rectosigmoid and anterior ampullary parts of rectum doesn’t bring any technical difficulties, and possibility of fulfillment a complete intraoperative visualization of local and lymphogenic spreading of cancer allows to keep all the principles of oncologic radicalism preliminary ligation of arteries and veins, separation of the tumor only by sharp way, minimal contact with tumor (“no touch” principle).
Conclusion
Expansion of indications for organ-preserving operations must be in parallel with the development of clear criteria for their fulfillment based on comparative analysis of long-term effects of the treatment, frequency of local recurrences, mastering and introduction of suturing devices, combined and complex curative programs, increasing ablativity of surgical interventions.
Thus, implementation of anterior resection of rectum with standard and extended lymph nodes dissection in the absence of contraindications is the most preferable method of surgical treatment in patients with stage II and III of the disease. Preference of low anterior resections with extended lymph nodes dissection is demonstrated in comparison with abdomino-anal resection of rectum in following indices: decrease of the number of recurrences, augmentation of life duration, improvement of indices of physical and psychical health.
References
1. Aschele C, Lonardi S. Multidisciplinary treatment of rectal cancer: medical oncology. Ann. Oncol. 2007, 18 (11) p1908-15.
2. Billingham B.P. Extended lymphadenectomy for rectal cancer: cure vs quality of life. Int. Surg. 1994, 79 (1) p11–22.
3. Cordon P.H., Nivatvongs S. Principles and practice of surgery for the colon, rectum, and anus. Second Edition. -St. Louis., Missouri, 1999. p994.
4. Engstrom P.F. Colorectal cancer. Clinical Oncology. 2000, 37, p361-70.
5. Greenlee R.T., Hill-Harmon M.B., Murray T., Thun M. Cancer Statistics. Cancer Jю Clin. 2001, 51 (1) p15-36.
6. Hobday T.J., Erlichman C.: Colorectal Cancer. In: Prognostic Factors in Cancer. 2nd ed. Ed. Gospodarowicz M.K. et al. –N.Y.: Wiley-Liss. 2001, p267-79.
7. Kalganov I.D., Zhouchenko А.P., Filon А.F., Moscalev A.I. Peritoneal micro dissemination of colon cancer. Annals of Oncology. 2006, 45, p121.
8. Lee S.I., Park Y.A., Sohn S.K. A survey on the impact of operation volume on rectal cancer management. J. Korean Med. Sci. 2007, 22 (Sl) S86-90.
9. Nicholls R.J., Tekkis P.P. Multidisciplinary treatment of cancer of the rectum: a European approach. Surg. Oncol. Clin. N. Am. 2008, 17 (3). p533-51.
10. Prete F., Prete F.P. Evolution of surgery for cancer of the anorectal junction. Chir. Ital. 2007, 59 (6) p763-70.
11. Soreide O., Norstein J. Rectal cancer surgery. –Berlin, Heidelberg: Springer. –Verlag, 1997, p164–80.
12. Troitskiy A.A., Tsarkov P.V. Preserving surgery for rectal carcinoma. Hepato-gastroenterology. 2006, 53 (S1) p51.
13. Ware J.E., Sherbourne C.D. The MOS 36-Item shortform health survey. Med. Care. 1992, 30(6) p473-83.
14. West of Scotland and Highland Anastomosis Study Group. Suturing or stapling in gastrointestinal surgery: a prospective randomized study. Br. J. Surg. 1991, 78, p337-41.
15. Wiklund I., Bardhan K.D., Muller-Lissner S., et al. Quality of life during acute and intermittent of gastroesophageal reflux disease with omeprazol compared with ranitidine. Results from a multicentre clinical trial. The European Study Group. Ital. J. Gastroenterol Hepatol. 1998, 30 (1) p19-27.
16. Wilke H., Stahl M. Colorectal cancer and metastasectomy: treatment of advanced disease. Annals of oncology. 2000, 11, p 45-49.
17. Zhouchenko А.P., Kalganov I.D., Filon А.F., Moscalev A.I. Cytoreduction for colon cancer with peritoneal dissemination
Correspondence to:
Behzod Navruzov
NATIONAL CANCER CENTER OF UZBEKISTAN
383, Farobi street, Tashkent, 100174, Uzbekistan
email: behzodn@mail.ru
Tel: +99871 227-13-27, 246-05-13
Fax.: +99871 227-15-96, 246-29-78

