S.N. Navruzov, N.F. Krotov, R.V.Khairutdinov
Republican Research Oncology Center of the Ministry of Public Health, Republic Uzbekistan
Abstract
Aims
The purpose of this work performed on the basis of the Republican Oncological Research Center (RORC) of the Ministry of Health of the Republic of Uzbekistan was to study the value of diagnostic videolaparoscopy (DVL) and videothoracoscopy (DVT) in the determination of invasion and resectability of EC and CEC; to analyze information ability of DVL and DVT and to compare their efficacy with ultrasonography and computed tomography.
Patients and Methods
Analysis of the results of clinical examination and surgery of 138 patients suffering from esophageal carcinoma was conducted. The patients were divided into 2 groups according to the applied diagnostic methods: 67 patients were in control group, and 71 – in the study group. The protocol of clinical examination in control group included ultrasonic investigation and computed tomography, and for studied group diagnostic video laparoscopy (DVL) and diagnostic video thoracoscopy (DVT) were added to the protocol.
Results
Comparative analysis of USG, CT, DVL and DVT findings during determination of resectability showed the following results. USG showed correct respectability in 89 (65.9%) patients out of 135 and was excluded in 11 (8.1%) patients. Ct allowed correct identification of respectability in 24 (38.7%) cases out of 61, negative results were noted in 13 (21.0%) cases. During DVL resectability was determined correctly in 31 (60.8%) patients, and non-resectability – in 16 (31.4%); in use of DVT respectability was established in 15 (75%) and excluded in 3 (15.0%) cases. Informational potential of USG was found as 74.1, CT – 59.7, DVL – 92.2 and DTV – 90.0%.
Conclusion
Advanced protocol of clinical examination allowed to adequate definite the prevalence and respectability of malignant process. Respectability increases up and frequency of repeated explorative operations significantly decreases due to including DVL and DVT into the protocol of clinical examination.
Keywords
Esophageal cancer, Cardioesophageal cancer, Diagnostic techniques
Introduction
The available diagnostic methods of esophageal cancer (EC) and cardioesophageal cancer (CEC) are not always potential to determine regional and total spreading of the process and resectability of the tumor and, consequently, the results of treatment remain to be unsatisfactory 2,3,9,10. Unavailing efforts of the conservative therapy and poor prognosis of disease in esophageal cancer and cardioesophageal cancer result in use of operative interventions as leading method of treatment 1,11. According to he data of many authors 5,6,7,8 in spite of advances achieved in the modern medicine in EC and CEC resectability fluctuates in range 36,6-67,6%. In this connection the role of precising diagnosis of tumor process distribution and evaluation of resectability of the tumors of this localization is significant.
Videoendoscopic technique widely used in the surgical practice has been introduced more and more frequently into the oncological clinics and used as diagnostic and therapeutic-diagnostic method 4, 12.
Patients and methods
The work was carried out on the basis of the analysis of the results of study and surgical treatment of 138 patients with EC and CEC admitted to the RORC during the period from 1997 to 2004. The patients were divided into 2 groups according to the methods of investigation used. The group 1 (control) included 67 patients; group 2 (study) consisted of 71 patients. In the study group additionally to the common diagnostic methods used in the control group (USG, CT) there were included DVL and DVT.
The mean age of the patients was 58.0+1.4 years in group 1, and 56.7+1.1 in group 2. The age diapason was from 23 to 78 years and from 25 to 70 in group 1 and 2, respectively. Among the patients the men prevailed – 90 (65.2%) in comparison with women 48 (34.8%), the ration was 2.19:1 in group 1 and 1,73:1 – in group 2.
Results and Discussion
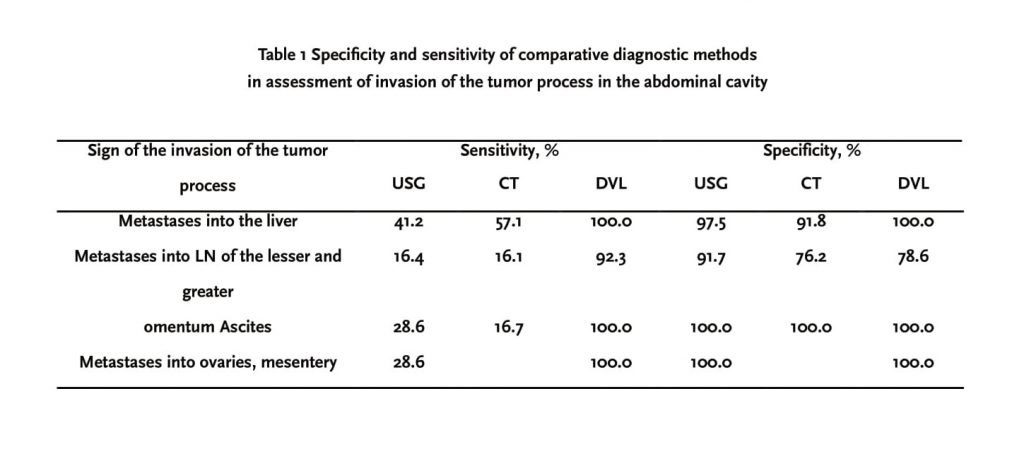
The technique of DVL allows evaluation of the state of the primary tumor, regional lymph nodes (LN), to reveal metastases of EC and CEC in the remote organs. The findings of investigations indicated that the results of DVL were significantly better than the results of ultrasonography (USG) and CT. Thus, according to these findings the DVL is the method of choice for identification of metastases in the liver, characterized by the high values of sensitivity and specificity (p<0.001); sensitivity of USG and CT in relation to identification of metastases in the liver was not high; however, both methods had sufficiently high specificity (Table 1). During evaluation of the criteria of metastasizing in the lymph nodes of the lesser and greater omentum the DVL sensitivity was reliably higher, than CT (p<0.01) and USG (p<0.05); however, USG specificity was higher (p<0.010, than that in CT and DVL (Table 1).
The study of information specificity of instrumental methods for determination of lymphogenic metastases in the paraaortal and retroperitoneal lymph nodes appeared to be also important. However, it should be noted that comparison of USG and CT with DVL is impossible because laparoscopy cannot give visual characteristic of this group of the lymph nodes. During determination of the diagnostic efficacy for identification of this group of lymph nodes the USG sensitivity (14.9%) in comparison with CT (60.00%, P<0.001) is lower. However, both methods have high specificity: USG – 93.0 and CT – 92.1%.
The refusal of surgical intervention is frequently connected with identification of the dissemination of the tumor process in the peritoneal cavity. DVL allowed identification correctly this sign in all the cases (9 patients). During diagnosis of ascites USG sensitivity was higher than CT (p<0.05), but considerably lower than DVL (p<0.001). However, it should be noted that all three methods had equal high specificity. During evaluation of the criteria of the removal metastasizing (ovary, mesocolon, intestinal mesentery) sensitivity of DVL was higher (p<0.001), than USG (100.0 vs.28.6%) in the similar high specificity (Table 1).
During tumor invasion into the liver and lesser omentum the parameters of information specificity of this method were not measured because of absence of true positive results of USG. The comparative analysis of the results of DVL and CT showed that sensitivity, specificity, and accuracy of DVL was reliably (p<0.005) higher than CT (Table 2). At the same time during determination of the tumor invasion into diaphragm the Ct sensitivity was higher than DVL (p<0.05); however, specificity of DVL was higher, though this difference was nit significant. It was established that DVL accuracy was also higher (p<0.01) than CT (Table 2). In cases of tumor invasion into the posterior wall and adjacent organs and structures (pancreatic gland, retroperitoneal fat, celiac trunk, abdominal aorta) the CT sensitivity (42.9%) was higher (p<0.001), than USG (6.9%); but specificity of CT was lower: 75.0 and 90.3%, respectively (p<0.05). Because of impossibility of visual assessment of the tumor invasion into the posterior wall during laparoscopy the comparison of information specificity of this method with methods USG and CT was not carried out.
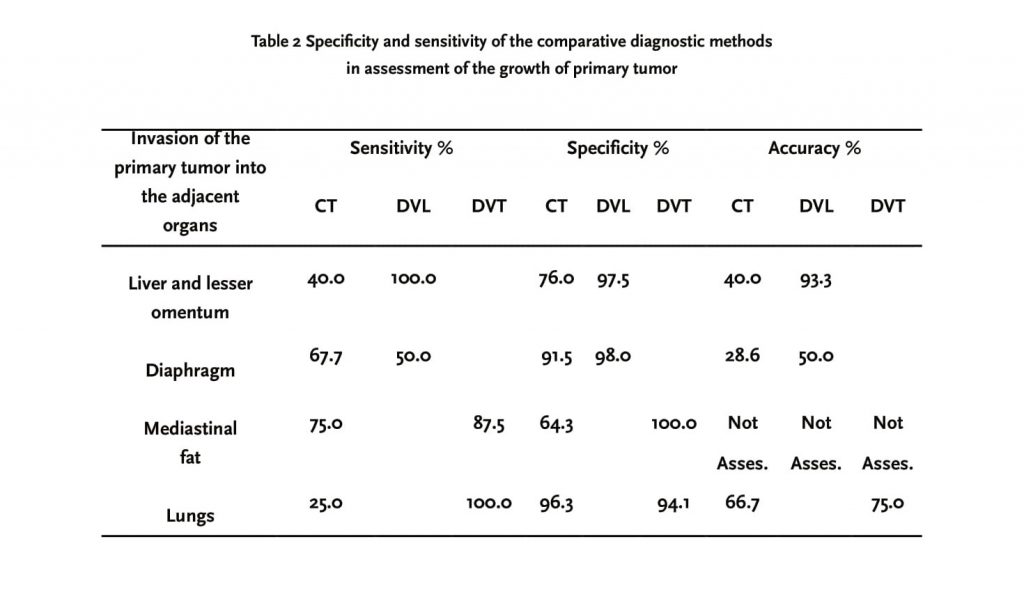
The tumor invasion into the organs and tissues of the chest in esophageal cancer may be the important sign characterizing tumor process. During determination of this sign of distribution in many patients the complications occurred which may be connected with the patient constitution, having previously irradiation therapy, duration of disease and others. During identification of the tumor invasion into the mediastinal fat it was found that parameters of sensitivity and specificity (p<0.05) of CT method was worse than those in DVT. The important diagnostic and prognostic criterion for advanced process is tumor invasion into the structures of the roots and/or parenchyma of the lungs. Measurement of this criterion of invasion showed that CT sensitivity was reliably (p<0.01) lower than sensitivity of DVT. However, the values of specificity and accuracy of CT were approximately equal those in DVT (Table 2). Comparative evaluation of diagnostic potentiality showed that sensitivity of DVT at whole was higher (p<0.01), than CT – 75.0 vs.33.3%. The difference in the parameters of specificity was not very big: CT – 88.0, DVT – 93.8%. The accuracy of CT method was reliably (p<0.001) lower than DVT – 14.3 vs.75.0%. During determination of the sizes of paraesophageal lymph nodes the sensitivity of the methods accounted for: CT – 70.6; DVT – 85.7%; specificity – 87.2 and 92.3%; accuracy – 70.6 and 85.7%, respectively.
Comparative analysis of USG, CT, DVL and DVT findings during determination of resectability showed the following results. USG showed correct resectability in 89 (65.9%) patients out of 135 and was excluded in 11 (8.1%) patients. CT allowed correct identification of resectability in 24 (38.7%) cases out of 61, negative results were noted in 13 (21.0%) cases. During DVL resectability was determined correctly in 31 (60.8%) patients, and non-resectability – in 16 (31.4%); in use of DVT resectability was established in 15 (75%) and excluded in 3 (15.0%) cases. Informational potential of USG was found as 74.1, CT – 59.7, DVL – 92.2 and DTV – 90.0%.
On the basis of results obtained there were calculated indices of sensitivity, specificity and accuracy.
According to these data, the method of choice for determination of invasion stage of tumor process in the abdominal cavity and resectability assessment in EC and CEC seemed to be DVL characterized by higher parameters of sensitivity- 96.9%, specificity – 84.2, and accuracy – 91.2% in comparison both with method of USG (89.0, 31.4, 78.8, respectively) and CT (54.5, 72.2, and 82.8%, p<0.001, respectively). The results of comparative analysis of diagnostic potentiality of DVT and CT in determination of EC resectability showed that DVT sensitivity was higher (p<0,001) than CT (93.9% vs.54.5%). DVT had higher specificity (75.0%) in comparison with CT (72.2%), the difference between parameters of specificity was insignificant.
During determination of resectability of EC and CEC, the lower specificity in our study was found in USG – 31.4% (p<0.001). However, taking into account high values of sensitivity (89.0%) and accuracy (78.8%) of USG its non-invasive character and absence of adverse effect the use of this method for diagnosis of the long-term metastasizing in EC and CEC is justified.
DVL and DVT are methods of high efficacy, information capacity of which is significantly increased than capacities of USG and CT. The performance of DVL in 51 patients allowed avoidance of explorative laparotomy in 15 (29.4%) patients. On the basis of the results of laparoscopy the attempts of radical intervention were taken in 36 patients. Out of them one intervention was explorative, the rest 35 patients were performed different types of resections. Resectability in the patients undergone radical operative interventions after DVT accounted for 97.2%. Performance of DVT to the patients allowed avoidance of explorative interventions in 15.0% of cases. Resectability in the patients who underwent to radical operative intervention after DVT was 94.1%.
The group 1 the total parameter of resectability (that is the ratio of the number of resections to the whole number of patients received operative treatment) accounted for 37.3%, and in group 2 – 81.3%. At the same time in group 2 of patients the number of explorative interventions was reliably less than in group1 (1.4 vs. 25.4%). It should be noted that in this group the radical surgical intervention was carried out in 53 (74.6%) out of 71 patients. Of them 52 were resections. Resectability (in relation to the number of patients who was performed radical surgical intervention) accounted for 98.1%.
Conclusions
1. During determination of invasion of EC and CEC in the abdominal cavity and assessment of resectability the method of choice – DVL is characterized by higher sensitivity, specificity, and accuracy in comparison with USG and CT.
2. Analysis of the parameters of diagnostic efficacy of DVT and CT showed reliable advantage of DVT in specificity, sensitivity, and information capacity in determination of EC resectability.
3. During determination of prevalence degree of EC and CEC the potentialities of the traditional methods in investigation, particularly CT and USG, are limited; diagnostic information capacity of USG accounts 74.1, and CT – 59.7%.
4. Information capacity of DVL in determination of local and remote distribution of the tumor process into the organs and structures of the abdominal cavity was noted in 92.2%. During identification of the direct markers of esophageal lesions and determination of the local invasion of EC and CEC the information capacity was 90.0% of cases.
References
1. Akahoshi K, Chijinwa Y, Hamada S, et al. Endoscopic ultrasonography: A promising method for assessing the prospects of endoscopic mucosal resection in early gastric cancer. Endoscopy. 1997; 29(7): 614-9.
2. Caletti GC, Ferrari A, Fiorino S, et al. Staging of esophageal carcinoma by endoscopy. Endoscopy 1993; 25(1): 2-9.
3. Chernousov A.F., Bodopolskiy P.M., Kurbanov F.CS. Esophagial surgery. //Moscow. – Medicine. -2000. – p. 350.
4. Davidov M.I., Aksel E.M. Malignant tumor in Russia and CIS in 2000. //M., ROSC named after Blohin N.N. RAMC. 2002. – p.281.
5. Flamen P., Lerut A., Van Cutsem W. et al. Utility of Positron Emission Tomografy for the staging of patients with potentially operable esophageal carcinoma. J. Clin. Oncol. 2000; 18: 3202-3210.
6. General Thoracic Surgery / Ed by Thomas W. Shields. – William@Wilkins. -1994, Vol.1 –1840p., Vol.2-1816p.
7. Glenn T.F. Esophageal cancer. Facts, figures, and screening // Gastroenterol. Nurs.2001; 24(6): 271-273.
8. Haraguchi Shuji, Koizumi Kiyoshi, Kawamoto Masashi et al. Video-assisted thoracoscopic excision of a benign cystic mesothlioma of pleura. Jap.J.Thorac. and Cardiov.Surg.1998; 46(8): 664-666.
9. Hashimoto H, Mitsunaga A, Suzuki S, et al. Evaluation of Endoscopic Ultrasonography for gastric cancer Tumor and presentation of Thro dimensional Display of Endoscopic Ultrasonography. Surg. Endosc. 1989; 3(4):173-81.
10. Inada T, Ogata Y, Andon J, et al. Significance of para-aortic lymph node dissection in patients with advanced and recurrent gastric cancer. Anticancer Res. 1994; 14(2B): 677-82.
11. Li S.D., Mobarhan S. Association between body mass index and adenocarcinoma of esophagus and gastric cardia. Nutr. Rev. 2000; 58(2P+1): 54-6.
12. Lightdale C.J., Winawer S.J. Screening diagnosis and staging of esophageal cancer. Semin. Oncol. 1984; 11(2): 101-12.
Correspondence to:
Dr. R.V. Khairutdinov
The Republican Research Oncology Centre
Farabiy 383, Tashkent city, Republic of Uzbekistan
Tel. +998971034026

