Qing Lin*, Jing Gong, Dongjun Yang, Yan Zhou, Chunyang
Li, Xianfeng Sun, Zhiqiang Cao
Department of Thoracic Surgery, The 1st Hospital of Yichun, Yichun, Heilongjiang Province 153000, China
ABSTRACT
OBJECTIVE To study surgery treatment strategies and outcomes in stage IIIA NSCLC (No pleural effusion) with adjuvant PandiMex naturopathic therapy.
METHODS Retrospective case studies on lung cancer surgery procedures and N2 mediastinal lymphadenectomy over the past 15 years, including 31 cases of Pneumonectomy (1 case of PandiMex preoperative neoadjuvant and PandiMex postoperative adjuvant therapy), 241 cases of right lung lobectomy (upper lobectomy 166 cases, 1 case of PandiMex preoperative neoadjuvant, medium lobectomy 5 cases, lower lobectomy 69 cases), 165 cases of left lung lobectomy (upper lobectomy 113 cases, lower lobectomy 51 cases, 1 case of PandiMex preoperative neoadjuvant), 32 cases of bronchial sleeve resections (sleeve right upper lobectomy 16 cases, sleeve left upper lobectomy 7 cases, medium and lower lobectomy + sleeve resection of main stem bronchus + sleeve right upper lobectomy bronchoplasty 9 cases), 36 cases of pulmonary arterioplasties with upper lobectomy (Tangential pulmonary artery resection 25 cases, wedge resection of pulmonary artery 11 cases), 6 cases of double- sleeve resection (right upper lobectomy with right sleeve pulmonary arterioplasty 1 case, left upper sleeve lobectomy bronchoplasty with left sleeve pulmonary arterioplasty 5 cases).
RESULTS 1 case (0.2%) developed chylothorax, 35 cases (6.8%) developed atelectasis and/or pneumonitis, 23 cases (4.5%) developed arrhythmia, 2 cases (0.39%) developed bronchial pleural fistula. No peri-operative deaths were observed. The one-year, three-year, five-year, and 10-year survival rates were 75%, 65%, 22% and 3.4% respectively.
CONCLUSION Radical resection and extended radical resection procedures can be performed for stage IIIA NSCLC without pleural effusion. It was proven to be safe as long as the surgical procedures were technically demanding. Sleeve resection is favor of avoiding pneumonectomy in some cases and provides much safer procedures for senior and cardiopulmonary dysfunction patients. Currently, the most effective treatment strategies employ combined modalities, including surgery for a patient with stage IIIA NSCLC N2 disease. PandiMex, a safe and reliable naturopathic adjuvant therapy, is an integral part of the multimodal approach.
KEY WORDS Stage IIIA Non-Small Cell Lung Cancer (NSCLC); Sleeve resection; Pneumonectomy; Lobectomy; Adjuvant therapy; PandiMex
INTRODUCTION
Currently, pulmonary resection is the treatment of choice for a majority of NSCLC patients with N2 disease. However, the radical operation is often technically more demanding in terms of effectiveness. Pulmonary resection is the most effective treatment approach and the most successful treatment strategies employ multimodality therapy, including surgery for patients with stage IIIA NSCLC without pleural effusion. The use of PandiMex in a multimodality regimen as neoadjuvant and adjuvant naturopathic therapy is likely to be a new option for a positive effect on survival. It is the aim of this article to describe surgery treatment procedures, complications as well as advantages of PandiMex adjuvant therapy in a retrospective study on 511 cases pulmonary resection for NSCLC patients with N2 diseases performed between March 1990 and April 2005.
DATA AND SURGICAL TECHNIQUES
Data
We studied 511 cases, which were 315 cases of male and 196 cases of female, age from 45 to 75 years old at the average of 65.2 years old. There were 408 cases (80%) of central lung cancer and 103 cases (20%) of peripheral lung cancer. Histological study confirmed 255 cases (50%) of squamous cell carcinoma, 133 cases (26%) of adenocarcinoma and 123 cases (24%) of adenosquamous carcinoma that all patients were at stage IIIA without pleural effusion.
Surgical Technique
Standard posterolateral thoracotomy incision was employed. Surgery Procedures: pulmonary vein (preventing from distant metastases), pulmonary artery, bronchus (prior dissection when necessary), mediastinal lymph nodes were involved subsequently. 65 cases of ligation of pulmonary vein and intrapericardial ligation of pulmonary vein were performed. The pericardium was incised longitudinally when phrenic nerve dissected free and pericardiotomy can be extended about 5-7cm around the pulmonary vein ligament, 1/3 atriotomy was considered when necessary and anastomosis (end-to end suture) was performed while auricle forceps is placing to prevent from unexpected bleeding. For the patients with pulmonary artery lesions, 25 cases of tangential pulmonary artery resection, 11 cases of wedge resection of pulmonary artery and 6 cases of double-sleeve resection of pulmonary artery were performed with interrupted monofilament absorbable 4/0 sutures. After completion of the anastomosis, thrombosis and occlusion is unlikely to occur when the gap is not less than 1/3 of pulmonary artery. 32 cases of bronchial sleeve resections were performed, including 16 cases of right upper sleeve lobectomy, 9 cases of sleeve resection of right main bronchus + medium and lower lobectomy + right upper sleeve lobectomy, 7 cases of left upper sleeve lobectomy, as well as 6 cases of double sleeve resection (sleeve resection of pulmonary artery + bronchial sleeve resection). Accurate anatomic resection is essential in sleeve resection, while the anastomosis was performed by running sutures at the cartilaginous part and tight the knots on the outside of sutures at an interval of 2 mm. All sutures were well done without leakage. Bronchial sleeve lobectomy is suitable for central lung cancer.
The main bronchus is transected. Frozen section of resection margins is performed. The lobe with part of the main bronchus is removed. The bronchial anastomosis is performed around 3-5 sutures in the inferior membrane with an interval of 2 mm. Mediastinal lymphadenectomy was performed in all treatment groups including adipose tissues and inspection of mediastinal lymph node lesions and distant metastases was revealed that the epithelium linings of superior vena cava, azygos vein, Internal thoracic artery and vein, pulmonary artery trunk, pericardium, pulmonary artery and aortic arch have certain degree of lesions and adhesions. Since using of sharp decollement, visual and finger inspection, electric knife are common safe procedures, not only swelling lymph nodes can be removed completely, but also cancer lymphangitis and peripheral tissues can be treated by high temperature electric knife.
Lower lobe is mobilized with extended subcarinal lymph nodes (level 7) dissection. However, posterolateral directed contralateral bronchus, anterior directed to pericardium and posterior directed to esophageal, upper to anterior sub-carina where 1-2 arteries attachments for blood supply, first the ligation of blood vessels need to be done, then the intervention of removal lymph nodes (level 7) is feasible and safe. Attentions must be paid to protect esophageal, thoracic duct, azygos vein from accidental injury. N2 mediastinal lymphadenectomy was performed in all of 511 cases at an average of 12 nodes removal. No associated intraoperative vascular injury and esophageal injury were found. 3 cases were selected for preoperative neoadjuvant PandiMex therapy, no evidence showed surgery procedures are technically difficult.
RESULTS
No peri-operative deaths were observed. 2 cases (0.39%) developed bronchial pleural fistula, 1 case (0.2%) developed chylothorax, 35 cases (6.8%) developed atelectasis and/or pneumonitis, 23 cases (4.5%) developed arrhythmia. Follow-up studies showed the one-year survival rate was 75% (355 out of 473), 38 subjects were lost to follow-up and may be suspect death. 3-year survival was 65% (76/117), 3 patients with PandiMex adjuvant therapy are still alive in a follow-up time 1-1.5 years). 5-year and 10- year survival rates were 22% (18/25) and 3.4% (1/29) respectively. The last patient developed thyroid metastasis in 7 years post-operation and was treated by localized radiotherapy to a completely recovery and alive till now.
DISCUSSION
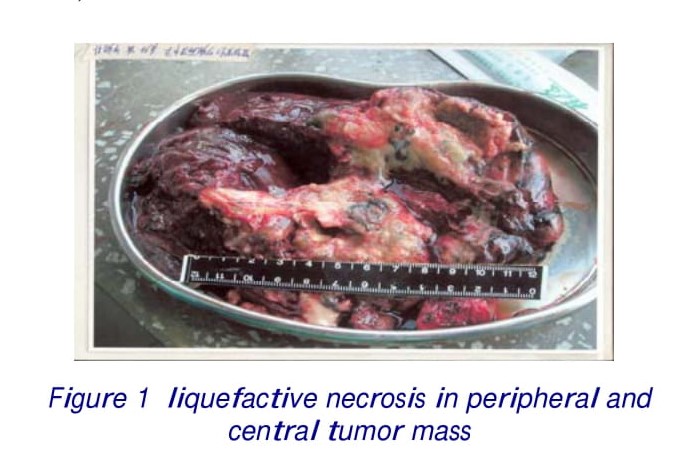
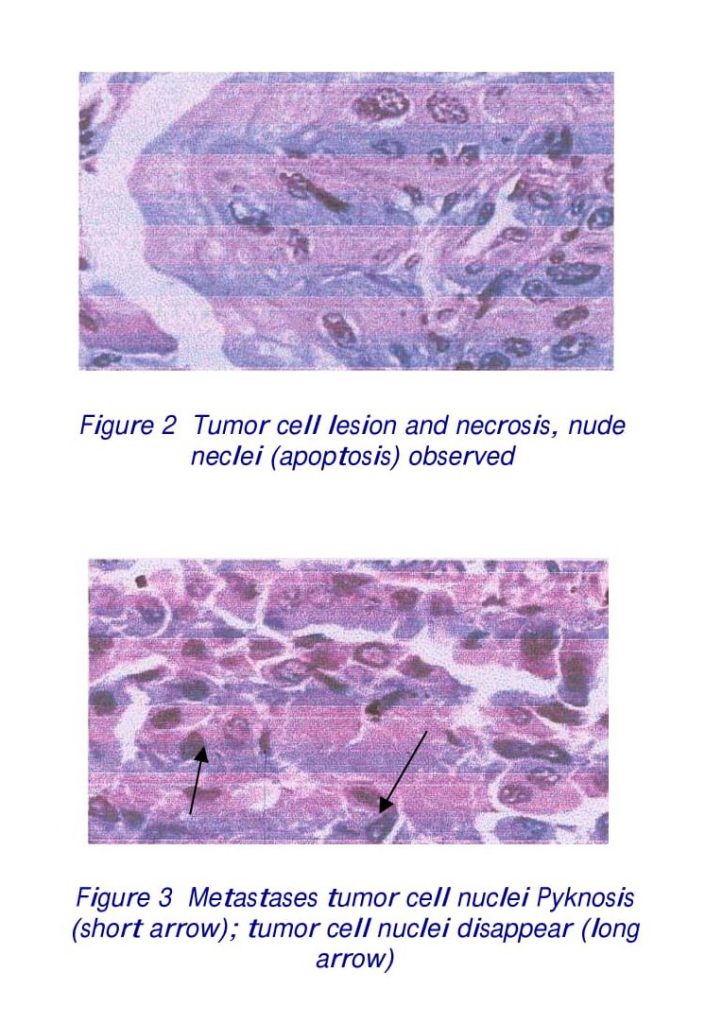
The incidence of lung cancer is increasing gradually in recent years. The advanced stage IIIA lung cancer at a time of diagnosis has become increasingly common due to no effective approaches available for early detection, early diagnosis, and early intervention of lung cancer. It has become common senses that the most effective treatment strategies employ multimodality therapy, including surgery for patients with stage IIIA NSCLC N2 diseases. Recent data suggest that the use of surgery with carboplatin neoadjuvant and adjuvant chemotherapy for patients with stage IIIA NSCLC N2 diseases improves patient’s survival. However, failure of chemotherapy has been observed due to its cytotoxic selectively but not exclusively single targeted mechanism, and development of chemo resistance in heterogeneous cancer cells. It is concerned that intra-operative risk and postoperative infection (immune deficiency) and atelectasis have been reported to be the most common early complications when inductive chemotherapy applied. To investigate tumor response and efficacy of large dosage of PandiMex naturopathic therapy for lung cancer, 3 cases of stage IIIA NSCLC patients were randomized selected for preoperative neoadjuvant PandiMex therapy, and in 1 case subsequently postoperative adjuvant PandiMex therapy is facilitated. During the surgery, softened tumor mass with partial liquefactive necrosis was observed (Figure 1). Only nude nuclei can be seen, or apoptosis of tumor cells were observed in lymph nodal metastases (Figures 2 and 3).
We believe that preoperative PandiMex neoadjuvant is applicable for:
1. Enhancement immune of stage IIIA patients to support vital to surgery procedures.
2. Avoiding common early complications of adhesion, infection and atelectasis and improvement of quality of life and a better recovery than surgery-alone patients.
3. Complete killing tumor cells and distal metastasis, further reduction the incidence of second primary lesions and significantly improvement 5-year survival rate.
4. One of the effective neoadjuvant therapies of choice incorporating surgery procedure by far.
Radical resection and extended radical resection procedures can be performed for stage IIIA NSCLC without pleural effusion. It was proven to be safe as long as the surgical procedures were technically demanding. The 5-year survival rate can reach 15-30%, inductive neoadjuvant chemotherapy can improve 5-year survival rate as much as 5%. Sleeve resection is favor of avoiding pneumonectomy in some cases and provides much safer procedures for senior and cardiopulmonary dysfunction patients. Currently, the most effective treatment strategies employ combined modalities, including surgery for a patient with stage IIIA NSCLC N2 disease. PandiMex, a safe and reliable naturopathic adjuvant therapy, is an integral part of the multimodal approach.
*Correspondence to: Qing Lin, MD
Email: l.q.05.02@163.com

