Steven Tucker, MD (USA), FACP (USA)
Prostate cancer is one of the most common causes of death in American men and is now the most rapidly increasing tumor in Singaporean men. In the 1980s, the prostate-specific antigen (PSA) test was introduced and has been widely used as a screening tool for prostate cancer. But PSA screening remains a controversial issue for one simple reason – there is still no direct evidence that PSA screening affects how long a man will live (i.e., survival). There are two very large ongoing randomized clinical trials hoping to answer this important question, but to date the results are not available. Thus, all published information on this topic comes from indirect or observational reports, which are considered less reliable than a major randomized and controlled study.
Physicians are often split over this complicated issue with urologists and cancer specialists in one camp and general practitioners and public health experts in another. Advocates for PSA screening describe the increased rate of early and potentially curable prostate cancers, a decrease in the number of men found with advanced prostate cancer and a global reduction in prostate cancer deaths (after PSA testing became common) as strong reasons to go ahead and recommend the test routinely. On the other side, it is well known that, unlike most other cancers, a very large number of cases of prostate cancer are not life-threatening; and therefore, PSA screening could lead to both over-detection and over-treatment of insignificant cancers (an oxymoron of the highest degree) resulting in high medical costs, serious permanent side effects, unexpected complications, and of course, lots of anxiety.
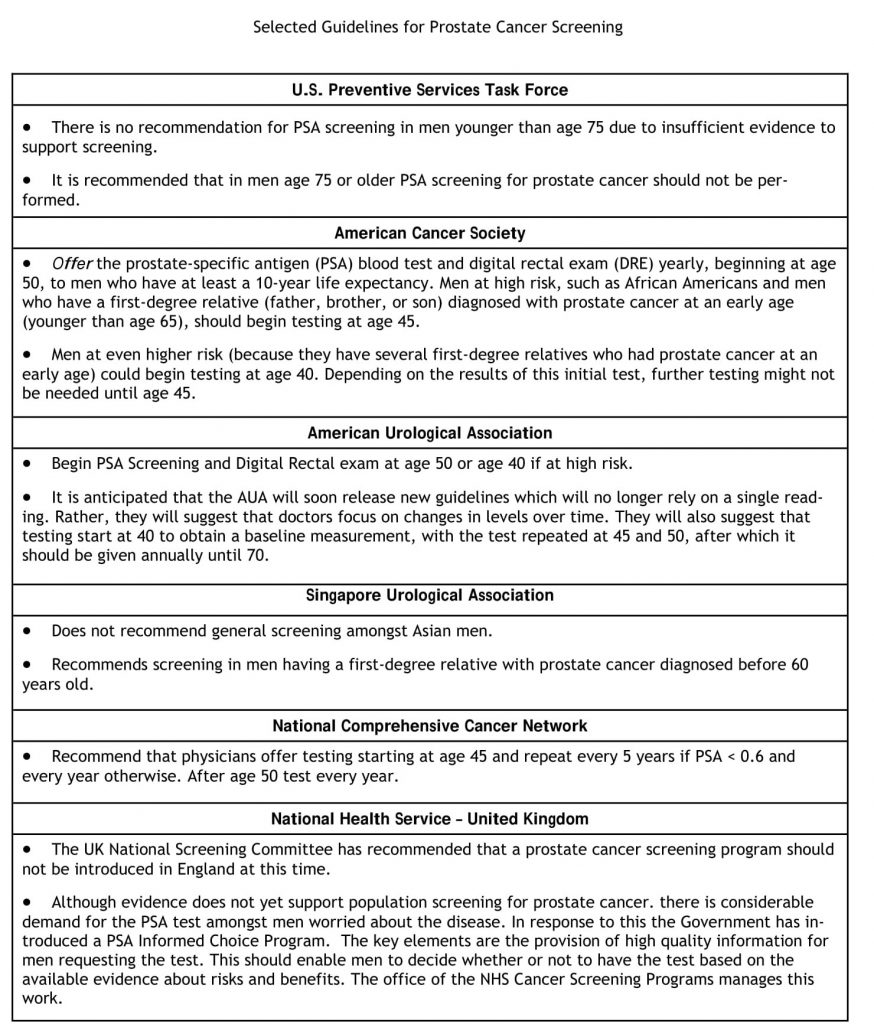
Consequently, there is a significant risk of doing more harm than good with PSA testing. Adding fuel to the fire, in August 2008, the respected U.S. Preventive Services Task Force issued new guidelines for doctors to stop PSA screening in men aged 75 and older. Although the recommendation is only for older men, it has reignited this passionate debate over the value of PSA screening in all adult men. The reason cited for this influential group’s recommendation is that evidence suggests the test does not help men over age 75. The panel still has not offered a guideline for men younger than 75 but believes there remains a lack of reliable evidence for or against screening in younger men.
Given that cancer is an emotionally charged topic for doctors and patients alike, let’s review some of the common arguments for and against PSA screening.
PSA Screening Advocate
PSA testing provides reassurance
While PSA testing may be challenged on its ability to selectively identify men with prostate cancer, it may serve more effectively at finding men who are at significantly lower odds of having cancer. Several studies have now shown that for men with a PSA level of less than 1 ng/ml, the lifetime risk of ever developing prostate cancer is very low, and for men with a screening PSA level of less than 0.5 ng/ml, the risk is even lower. Thus, the test may reassure many men who worry about prostate cancer.
Treatment is better when started early
Aside from the common-sense wisdom that early treatment is better than late, there is emerging data that early interventions in prostate cancer can make a meaningful difference. We now know that early use of hormonal medicines makes men with metastatic and high-risk prostate cancer live longer. Also, a recent study of surgery compared to watchful waiting reported a survival benefit with early surgery. Last, when we use predictive models in prostate cancer, those men with low PSA levels are reliably found to have the best outcomes in terms of relapse and surgical pathology.
Screening has resulted in “stage shift”
Screening results in a predictable shift with more cases presenting earlier for medical care. This observation has been published many times in prostate medicine and in other fields. In the 1980s, about 25% of all cases were advanced or metastatic, while today that number is closer to 5%. Not only do patients present with less cancer in the body, but the features of the cancer are also less aggressive.
Survival has improved in the PSA era
Prostate cancer survival rates (5-year rates) have significantly improved from less than 80% to 99% in the PSA testing era. The overall death rate from prostate cancer has been improving in both the USA and Europe since PSA screening become common practice.
PSA Screening Nihilist
The Gold Standard
The main and most important argument against prostate cancer screening is that quality evidence for the effectiveness of screening remains absent. The gold standard in medicine (and as evidence) is the result from a randomized prospective clinical trial. Two very large such trials of PSA screening began more than 15 years ago, but to date there are no results for or against screening. We are still in a scenario of uncertainty about this test as a screening tool.
Screening can be harmful (and expensive)
Harm from screening is well known; benefit from screening has yet to be shown. There are potential physical and emotional harms from PSA screening. After biopsy, men can develop serious infections, blood in urine or semen, chronic prostate pain, increases in PSA and unnecessary anxiety about further testing or diagnosis.
Aside from the harm of the screening and diagnosis (or over-diagnosis) process, there are even more serious harms from over-treatment. The common complications from treatment of prostate cancer include erectile dysfunction, incontinence, and bowel problems. These side effects are often permanent and emotionally crippling. When a patient with a screen-detected and indolent (non-aggressive) prostate cancer suffers permanent side effects such as these, it becomes clear that the potential harm can easily outweigh the potential benefit.
Prostate cancer is over diagnosed and over treated
Overdiagnosis leads to overtreatment. Recent studies of both surgery and active surveillance suggest that at least 20 men need to be treated with radical surgery to prevent one death from prostate cancer. This so-called “number needed to treat” is unknown in the modern PSA era but is expected to be significantly higher than 20:1. Given the costs and potential side effects, it would be better to wait for data on screening rather than use PSA screening today.
Numerous studies suggest the disease is “over-diagnosed” — that is, detected at a point when the disease most likely would not affect life expectancy — in 29% to 44% of cases. Prostate cancer often progresses very slowly, and a large number of these cancers discovered through screening will probably never cause symptoms during the patient’s lifetime, particularly for men in their 70s and 80s. At the same time, aggressive treatment of prostate cancer can greatly reduce a patient’s quality of life, resulting in complications, such as impotency and incontinence.
Improved Prostate Cancer Survival data is not due to Screening
Decreased deaths from prostate cancer are due to numerous factors, such as better and safer therapy (including surgery), the use of early therapy in advanced disease and new treatments in metastatic disease. It is clear that with improved techniques and more prostate surgeries being performed that the risk of peri-operative death or complications has fallen dramatically. Also, the improved survival rates may be a better reflection of increasing life expectancy in men across the USA and Europe. It should be noted that the decline in prostate cancer deaths is nearly equal in countries that routinely screen (USA) and in countries that do not (Netherlands).
The overall improvement in prostate cancer patients may also be a reflection of improved medicines, such as chemotherapy, early hormonal therapy and supportive therapy to prevent complications (e.g., bone targeted therapies). Even the use of other medicines, such as cholesterol lowering drugs, may contribute to the overall improvements in prostate cancer survival. It is clear that the decrease in deaths from prostate cancer worldwide are not solely due to PSA screening.
Summary
Overall, with PSA screening, you have a chance that the screening may help you live longer or better, but you also have a chance that the screening, detection and treatment may harm you. For patients at age 75, the chances are high that there will be more negative impact than positive from PSA screening. Recently, Swedish researchers collected 10 years of data on men whose cancer was diagnosed after the age of 65 and found no difference in survival among those who were treated for the disease and those whose cancers were monitored but treated only if the cancer progressed. The finding suggests that for most men, forgoing PSA screening at 75 is a safe option.
Given all of this conflicting information, I believe a reasonable approach is to provide a balanced discussion with older men. We never want to prevent a man from getting screening, but certainly they should be very well informed about the uncertainties. In my experience, there are always some men who say, “I expect to live to 100” or “I just need to know now.”
PSA screening remains controversial and while often considered “standard of care” for men over the age of 50, there is no direct level I evidence to support its use. While partisans in this debate await results of randomized trials, doctors in day-to-day care with patients need a practical approach. I advise that patients who want PSA screening should spend an extra 10 minutes or so with their doctor to review the pros and cons. The new guidelines from the U.S. Preventive Services Task Force also help us make a stronger argument against screening in men over the age of 75, but again, we should emphasize a personalized and individualized approach to this conundrum for each patient.
Correspondence to: Steven Tucker, MD (USA), FACP (USA)
Pacific Cancer Centre, Singapore Phone: (65) 6883-6968
Email: info@pacificcancercentre.com